
A repeat complete blood count was performed one hour after symptom onset which showed a hemoglobin of 10.3 g/dL and a platelet count of 103 x10 3 u/L. Additionally, uterine massage was performed to aid in hemorrhage control and the patient was administered IV oxytocin, methylergonovine maleate, carboprost, and vaginal misoprostol. Blood pressure was significant for systolic pressure of 80 mmHg. Following completion of the caesarian section, peak airway pressures normalized to less than 30 cmH 2O but end tidal CO2 levels remained as high as 52 mmHg despite hyperventilation. Albuterol and sevoflurane were subsequently utilized in an attempt to increase bronchodilation. However, end tidal C02 was elevated to 54 mmHg despite hyperventilation and peak airway pressures were elevated to 38 cmH 2O. First, a report of AFE requires a sudden onset of cardiorespiratory arrest, which consists of both hypotension (systolic blood pressure 90%. In 2016, uniform diagnostic criteria were proposed for reporting on cases of AFE.
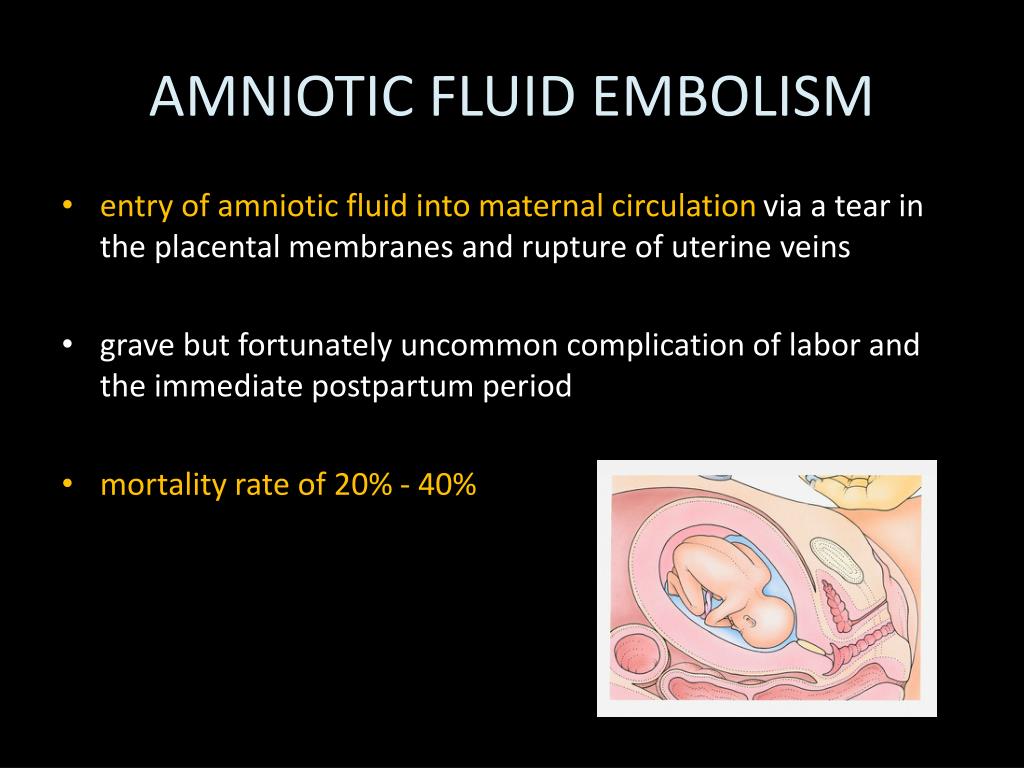
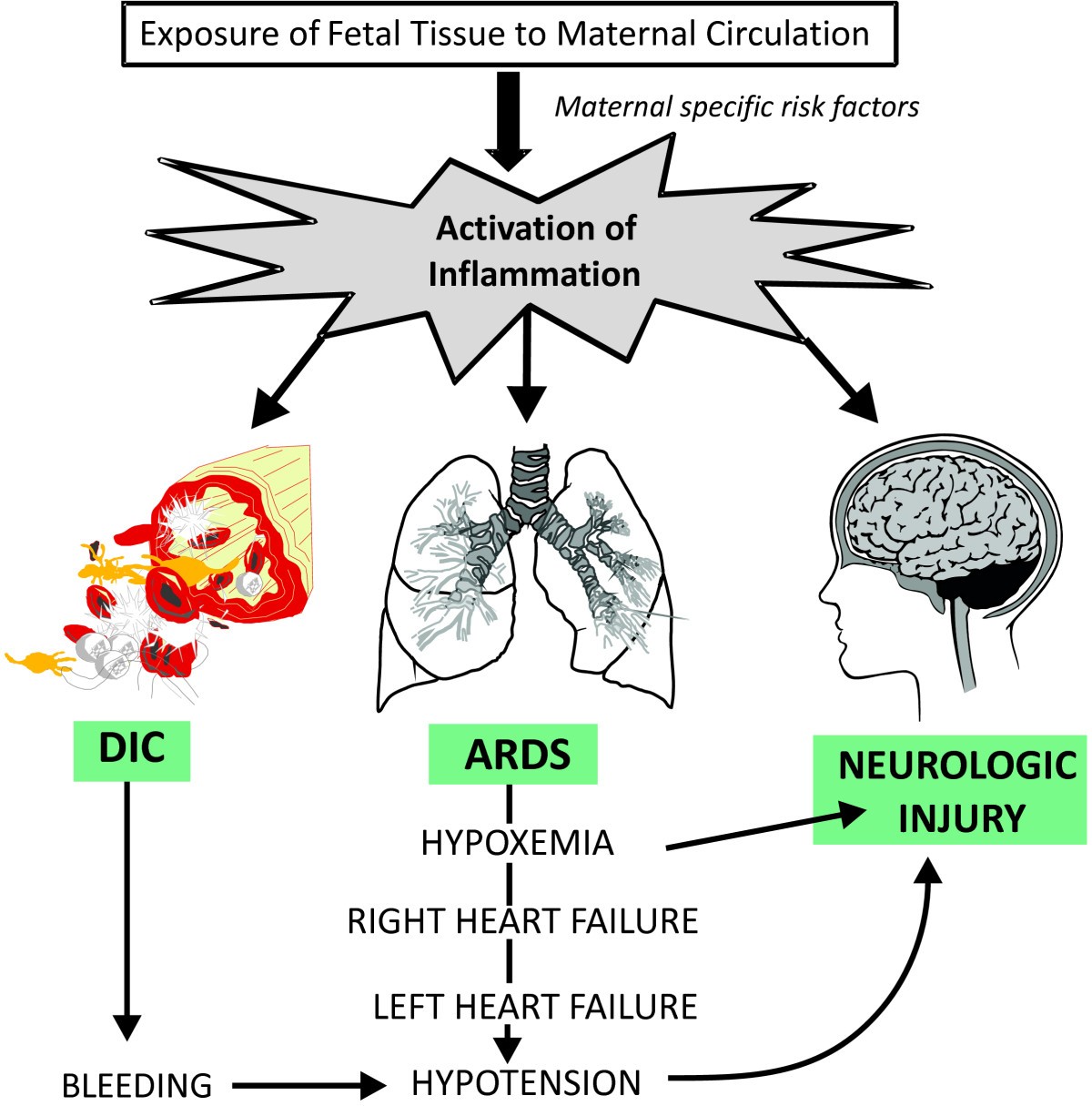
However, rapid diagnosis of AFE and immediate obstetric and intensive care has proven to play a decisive role in maternal prognosis and survival (7-9). Despite best efforts, it remains one of the leading causes of maternal death (1,5,6). Mortality rates vary but have been reported to range from 11% to more than 60%, with the most recent population-based studies in the United States reporting a 21.6% fatality rate (1-4). A literature review regarding the current recommendations for management of this condition follows as well as a proposed treatment algorithm.Īmniotic fluid embolus (AFE) is a rare and life-threatening complication of pregnancy a recent population-based review found an estimated incidence ranging from 1 in 15,200 deliveries in North America and 1 in 53,800 deliveries in Europe (1). The following case study demonstrates the importance of quick recognition as well as an interdisciplinary approach in caring for such a condition. 2012 256(3):476-86.Ryan J Elsey DO 1*, Mary K Moats-Biechler OMS-IV 2, Michael W Faust MD 3, Jennifer A Cooley CRNA-APRN 4, Sheela Ahari MD 4, and Douglas T Summerfield MD 1ĭepartments of Internal Medicine 1,Obstetrics and Gynecology 3,and Anesthesia 4Īmniotic fluid embolus is a rare and life threatening peripartum complication that requires quick recognition and emergent interdisciplinary management to provide the best chance of a positive outcome for the mother and infant. Admission rapid thrombelastography can replace conventional coagulation tests in the emergency department: experience with 1974 consecutive trauma patients. Holcomb JB, Minei KM, Scerbo ML, et al.TEG-guided resuscitation is superior to standardized MTP resuscitation in massively transfused penetrating trauma patients. Disseminated intravascular coagulation in obstetric disorders and its acute haematological management. How we treat: management of life-threatening primary postpartum hemorrhage with a standardized massive transfusion protocol. Burtelow M, Riley E, Druzin M, Fontaine M, Viele M, Goodnough LT.Gist RS, Stafford IP, Leibowitz AB, Beilin Y.Postpartum hemorrhage and transfusion of blood and blood components. Jansen AJ, Van rhenen DJ, Steegers EA, Duvekot JJ.Thromboelastographic goal-directed blood component therapy for severe hemorrhage.


 0 kommentar(er)
0 kommentar(er)
